Spring is nearly upon us and along with trees and flowers, seasonal allergies will bloom once again. Even though allergies can be annoying, debilitating and even life-threatening, the science behind them is fascinating. Science published a timely paper at the end of February describing some of the ways different kinds of allergens work. Allergens are small parts—individual proteins or molecules—of things that cause allergic responses.
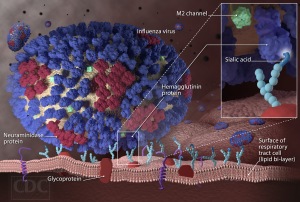
The group who published the study worked with cells called mast cells, one of the common types of the immune cells that respond to allergens and make you itchy, sneezy and swollen. Before they can activate mast cells, allergens have to be recognized by a particular type of antibody, or immunoglobulin, called immunoglobulin E, or IgE. On one end, IgE binds an allergen, and on the other it interacts with a protein receptor on mast cell surface.
By connecting the mast cell to the allergen, IgE gives the mast cell permission to do its thing, and its thing is called degranulation. Mast cells are brimming with packets, or granules, of histamine and heparin and other proteins that damage microbes as well as tissue. When the cells degranulate, they open up and release their contents into whatever tissue they happen to be in—the skin, the lungs or the gut for example. Many of the contents released make blood vessels leaky and attract lots of immune cells, causing inflammation. Antihistamines prevent the released histamine from binding its receptors on blood vessel cells. Another treatment option currently under investigation is a drug that blocks the interaction between IgE and the receptor on mast cells to prevent this process from even getting started.
The recent Science paper took a close look at the mast cell response to IgE-bound allergen and showed just how fine-tuned it can be. The researchers activated mast cells with allergens that bound tightly or weakly to IgE and found that the strength of the interaction, also called affinity, changed the way that mast cells responded.
The researchers could study mouse mast cells in culture dishes, because mast cells grow up from stem cells inside bone marrow. So they grew up mast cells from mouse bone marrow and then gave them the strongly binding allergen (high affinity) or the weakly binding one (low affinity). They could get the mast cells to respond and degranulate with both, but it took 100 times more of the weak binding allergen to get the same response caused by the strong one.
To understand how allergic reactions work in living creatures, researchers often sensitize mouse ears by exposing them to an allergen and later re-introduce the allergen through the bloodstream. Then they can measure how inflamed the ears get and how many and what kinds of immune cells travel to the ear after injecting the allergen. In this study, the strong binding allergen caused more intense and more sudden ear inflammation and immune cell infiltration than the weaker binding allergen.
So how does this fascinating mechanism actually relate to human allergies, which for some people is a life-threatening condition. Although some allergies go away with age, there is currently no permanent cure for those that don’t. Treatment of serious allergies is centered around desensitization immunotherapy, which is just repeated exposure to small doses of allergen over time. The treatment may last anywhere from months to a lifetime and there are no biomarkers, or biological tests, that tell doctors when the treatment is working. Instead, they simply test allergens on patients, which could mean pricking the skin or making them eat peanuts one at a time until they do or don’t get sick.
A clinical study that came out in January helped me understand how knowledge of allergen binding strength could be helpful in treatment. In this study, children with milk allergies were undergoing oral immunotherapy, which in this case simply meant they had to drink small amounts of milk that were increased over time. The researchers collected serum samples from the kids in the study and measured levels of IgE as well as the affinity of IgE for proteins found in cow’s milk to see if either would change as kids became more tolerant to milk.
In some cases, the immunotherapy had to be discontinued because the reactions to milk were too severe. The researchers found that the IgE from the kids whose treatment was discontinued bound more tightly to milk proteins compared to kids who responded well to the treatment. So the strength of the interaction between IgE and allergens does matter, at least in the case of cow’s milk allergies. This study didn’t look at mast cells, but it does indicate that the molecular details of how IgE connects allergens to mast cells are worth studying. Those details can provide clues about what is going on inside a person with allergies and how well they may respond to immunotherapy.
Sources:
Mastcellaware.com (A whole website about Mast Cells)
Suzuki R., Leach S., Liu W., Ralston E., Scheffel J., Zhang W., Lowell C.A. & Rivera J. (2014). Molecular Editing of Cellular Responses by the High-Affinity Receptor for IgE, Science, 343 (6174) 1021-1025. DOI: 10.1126/science.1246976
Savilahti E.M., Kuitunen M., Valori M., Rantanen V., Bardina L., Gimenez G., Mäkelä M.J., Hautaniemi S., Savilahti E. & Sampson H.A. & (2014). Changes in IgE and IgG4 epitope binding profiles associated with the outcome of oral immunotherapy in cow’s milk allergy, Pediatric Allergy and Immunology, n/a-n/a. DOI: 10.1111/pai.12186
Moran T.P., Vickery B.P. & Burks A.W. (2013). Oral and sublingual immunotherapy for food allergy: current progress and future directions, Current Opinion in Immunology, 25 (6) 781-787. DOI: 10.1016/j.coi.2013.07.011